LifWavNet: Lifting Wavelet-based Network for Non-contact ECG Reconstruction from Radar
Abstract: Non-contact electrocardiogram (ECG) reconstruction from radar signals offers a promising approach for unobtrusive cardiac monitoring. We present LifWavNet, a lifting wavelet network based on a multi-resolution analysis and synthesis (MRAS) model for radar-to-ECG reconstruction. Unlike prior models that use fixed wavelet approaches, LifWavNet employs learnable lifting wavelets with lifting and inverse lifting units to adaptively capture radar signal features and synthesize physiologically meaningful ECG waveforms. To improve reconstruction fidelity, we introduce a multi-resolution short-time Fourier transform (STFT) loss, that enforces consistency with the ground-truth ECG in both temporal and spectral domains. Evaluations on two public datasets demonstrate that LifWavNet outperforms state-of-the-art methods in ECG reconstruction and downstream vital sign estimation (heart rate and heart rate variability). Furthermore, intermediate feature visualization highlights the interpretability of multi-resolution decomposition and synthesis in radar-to-ECG reconstruction. These results establish LifWavNet as a robust framework for radar-based non-contact ECG measurement.
Sponsor
Paper Prompts
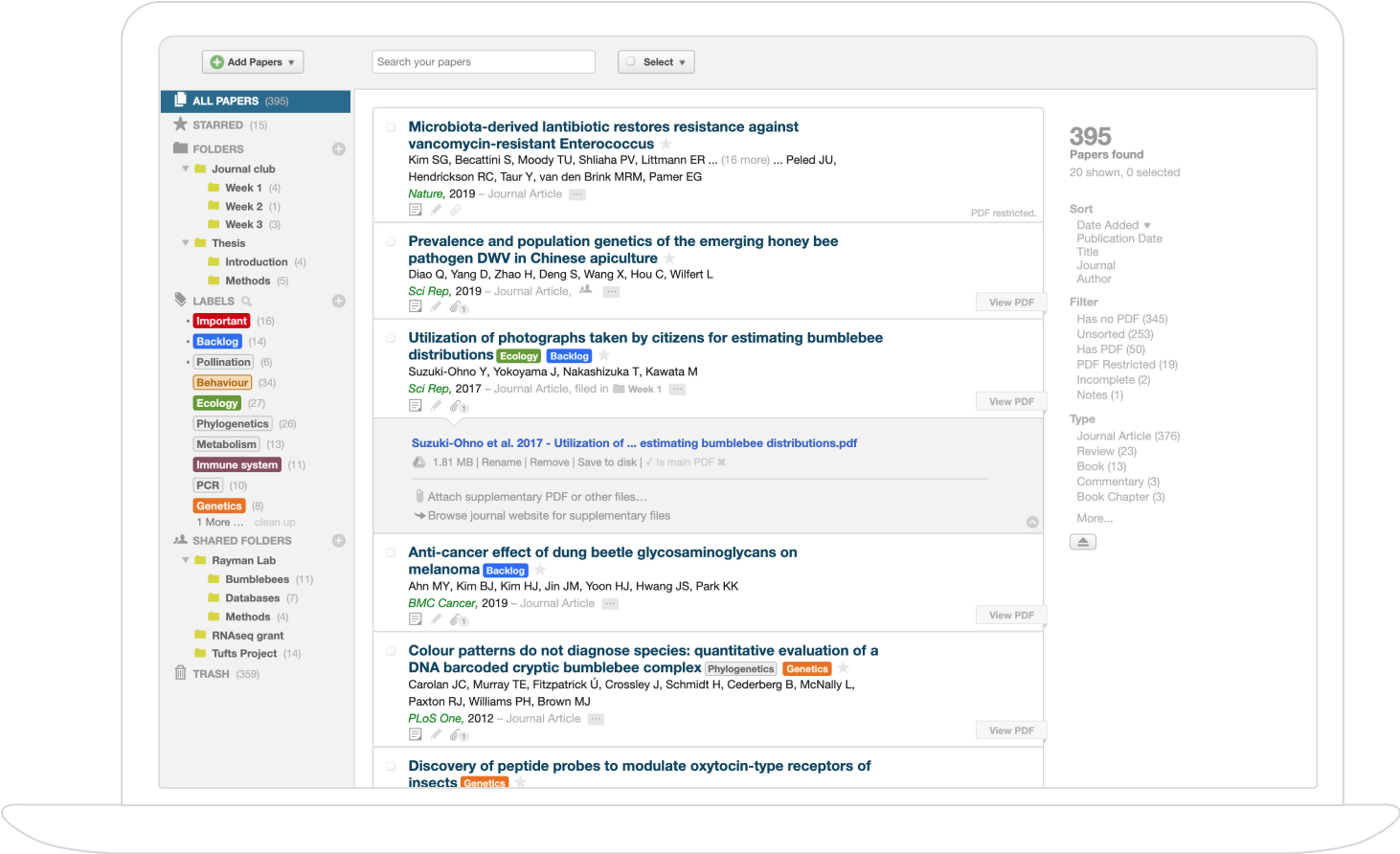
Sign up for free to create and run prompts on this paper using GPT-5.
Top Community Prompts
Explain it Like I'm 14
What this paper is about (big picture)
This paper introduces a new way to read the heart’s electrical signal (ECG) without touching the body. Instead of sticky chest electrodes, it uses a radar sensor that can “see” tiny chest movements caused by the heartbeat. The authors built a special AI model, called LifWavNet, that turns those radar signals into ECG waveforms—the classic P, Q, R, S, T shapes doctors use to understand heart health.
What the researchers wanted to find out
In simple terms, they asked:
- Can we reconstruct a full, accurate ECG from a contact-free radar signal?
- Can a smarter, “wavelet-based” model learn the right features from radar to capture all parts of the ECG (including the tricky P and T waves, not just the big R peaks)?
- Will this help measure heart rate (HR) and heart rate variability (HRV) reliably?
- Can we do it efficiently and in a way that is easy to understand?
How their approach works (explained with everyday ideas)
The method has three core ideas:
1) Radar-to-ECG with multi-resolution “wavelets”
- Think of the heartbeat like music: it has deep, slow parts (like the bass—breathing and P/T waves) and sharp, quick spikes (like the treble—QRS complex).
- “Wavelets” are like smart magnifying glasses that zoom into different parts of the signal: some look at slow changes, others at quick changes.
- The authors use a special kind of wavelet system called “lifting wavelets.” Unlike fixed tools, lifting wavelets can be learned and customized by the AI during training—like building the exact right tool from Lego pieces instead of using a one-size-fits-all tool.
2) Analysis and synthesis (break it apart, then rebuild)
- First, the radar signal is “analyzed” (broken into pieces) at multiple scales:
- Approximation parts: slow, smooth stuff (like breathing and P/T wave shapes).
- Detail parts: fast, sharp stuff (like the QRS spikes).
- Then, the model “synthesizes” (rebuilds) an ECG by combining these parts in the right way, guided by what true ECGs look like.
3) Matching in both time and frequency (like checking both the lyrics and the tune)
- Signals have a “time” view (waveform shape) and a “frequency” view (what pitches happen, when).
- They use STFT (Short-Time Fourier Transform), which is like analyzing the tune through windows of different lengths:
- Long windows capture precise pitch but blur timing.
- Short windows capture timing but blur pitch.
- The model uses multiple window sizes (multi-resolution STFT loss) so it learns both sharp beats (QRS) and smoother shapes (P and T waves), making the final ECG more realistic.
What they built (the LifWavNet model)
- LifWavNet is an end-to-end neural network designed around the multi-resolution idea.
- Inside it are “Lifting Units” that split features (like even/odd parts) and apply “predict” and “update” steps to separate smooth and sharp features—these steps are learnable (not fixed), using:
- Convolutions (good at spotting local patterns),
- Self-attention (helps the model focus on what matters across time),
- Channel attention (helps pick the most useful features).
- “Inverse Lifting Units” then carefully put the pieces back together to form the ECG waveform.
What they found and why it matters
- They tested LifWavNet on two real datasets:
- CR-RVS: clinical recordings with synchronized radar and medical ECG.
- Med-Radar: lab recordings with radar under the bed and ECG references.
- LifWavNet beat other advanced methods (RF2ESG and Air-ECG) on:
- ECG accuracy (stronger correlation with the true ECG, lower error),
- Heart rate (HR) and heart rate variability (HRV) measurements (lower mistakes in beats per minute and variability).
- It was also efficient enough to be practical—not slow or overly heavy.
- Bonus: The model is more interpretable. By visualizing the middle layers, you can see how it separates breathing-like parts from heartbeat spikes, then recombines them into a believable ECG. That’s useful for trust and medical relevance.
Why this is important
- Comfort: No sticky electrodes or wires—great for babies, older adults, burn patients, or anyone with sensitive skin.
- Convenience: Could enable long-term home monitoring without discomfort, and work in the dark (radar doesn’t need light).
- Accuracy: Getting full ECG shapes (not just beats) can help detect more heart issues.
- Reliability: Better HR and HRV estimates support stress tracking, fitness, and cardiac risk monitoring.
What this could lead to (future impact)
- Smarter non-contact heart monitors in homes, hospitals, and ambulances.
- Safer monitoring in places where touching patients is hard (e.g., infectious disease settings).
- Combining radar with other sensors for even better readings.
- More interpretable AI in healthcare—doctors and engineers can understand how the model uses signal features.
In short, LifWavNet shows that with the right “multi-scale” tools and a good learning strategy, radar can reconstruct detailed ECGs without touching the body, opening the door to comfortable, continuous heart monitoring.
Knowledge Gaps
Knowledge gaps, limitations, and open questions
Below is a single, concrete list of what remains missing, uncertain, or unexplored in the paper, aimed to guide future research:
- Dataset scope and diversity: evaluation is limited to two small datasets (30 and 9 healthy subjects), mostly in controlled settings; no patients with arrhythmias, structural heart disease, or other clinically relevant abnormalities are included.
- Subject-level generalization: the train/test split is described at the chunk level but not clearly at the subject level; potential leakage from the same subjects across splits undermines generalization estimates. A leave-one-subject-out or cross-subject validation is needed.
- Motion robustness: experiments are performed under quasi-static postures; robustness to random body movement, posture changes, coughing, talking, and ambulatory conditions remains untested.
- Respiration interference: while the method claims to separate multi-scale components, there is no quantitative analysis of respiration suppression or robustness under high respiratory amplitude or irregular breathing.
- Radar hardware variability: generalization across radar types (CW vs FMCW/UWB), frequencies (other than ~24 GHz), antenna configurations (single vs MIMO), mounting orientations, subject-radar distance, and environmental multipath/clutter is not evaluated.
- Clothing and bedding effects: Med-Radar recordings involve a radar under the bed; effects of different mattress materials, bedding layers, and clothing on reconstruction fidelity are not studied.
- Synchronization and deployment realism: CR-RVS uses sophisticated post-hoc synchronization (Gold code and clock drift correction); feasibility without ground-truth ECG for alignment in real deployments (no shared codes, clock drift) is not addressed.
- End-to-end from I/Q: the pipeline relies on radar-to-displacement pre-processing; the sensitivity of LifWavNet to errors in displacement extraction and its effectiveness when trained end-to-end directly from radar I/Q are unexplored.
- Sampling rate dependence: all signals are resampled to 200 Hz; the impact on morphology (e.g., QRS width, high-frequency components), and generalization across different sampling rates is not analyzed.
- Clinical metrics: evaluation focuses on Pearson correlation, MRE, HR, and RMSSD; clinically meaningful metrics such as R-peak detection sensitivity/PPV, fiducial timing errors (PR, QRS, QT), QTc, beat morphology similarity (e.g., DTW distance), and diagnostic performance (e.g., AF detection) are missing.
- HRV window length: RMSSD is estimated on 5.12 s segments; short windows can yield unstable HRV estimates; effects of longer windows and time aggregation strategies are not evaluated.
- Error acceptability: the clinical acceptability thresholds for HR and HRV errors (and waveform deviations) are not discussed; no comparison to clinical standards or physician assessment.
- Multi-resolution STFT loss design: window sizes (800, 400, 200 samples at 200 Hz) are chosen empirically without justification; whether learned windows, adaptive time-frequency losses (CWT/Stockwell), or beat-synchronous losses improve morphology is unknown.
- Phase handling in STFT loss: it is not specified whether the STFT loss is applied to magnitude only or complex spectra; implications for phase alignment and waveform fidelity remain unclear.
- Wavelet lifting properties: the learnable split/merge via strided conv/deconv lacks guarantees for perfect reconstruction, stability, or aliasing control; theoretical analysis or constraints (e.g., biorthogonality) are not provided.
- Parameter sharing and invertibility: prediction/update blocks do not share parameters between analysis and synthesis; the trade-off between flexibility and invertibility/consistency is not systematically studied.
- Interpretability quantification: while feature visualizations are shown, there is no quantification linking learned filters/components to physiological bands (e.g., QRS vs P/T), nor analysis of learned kernels’ frequency responses.
- ECC modeling: the approach does not explicitly incorporate excitation–contraction coupling or biophysical priors; whether hybrid physics-informed constraints improve cross-domain mapping is an open question.
- Personalization and adaptation: no investigation into subject-specific fine-tuning, transfer learning, or domain adaptation to new demographics and devices; fairness across sex, age, BMI, and chest anatomy is unexamined.
- Noise robustness: performance under additive noise, clutter, and interference (RF sources, multipath) is not analyzed; controlled stress tests (SNR sweeps) are missing.
- Failure case analysis: the paper lacks systematic characterization of failure modes (e.g., missed beats, distorted T-waves), conditions causing degradation, and mitigation strategies.
- Real-time deployment: runtime is reported, but streaming latency, memory footprint, and energy consumption on embedded hardware are not evaluated; suitability for on-device or bedside operation remains uncertain.
- Chunked processing: processing 5.12 s non-overlapping chunks may introduce boundary effects; strategies for overlap, windowing, and continuity in streaming ECG reconstruction are not explored.
- Amplitude calibration: signals are scaled to [-1, 1]; preservation of clinically meaningful amplitude (e.g., mV units) and baseline wander handling are not addressed.
- Cross-dataset transfer: models are trained and tested on combined datasets but the paper does not show train-on-one/test-on-another results; robustness to dataset/domain shift is unclear.
- Baseline breadth: comparisons are limited to two open-source methods; many cited approaches (U-Net, transformer/STFT, RSSRNet, WaveGRUNet, ODE-based) are omitted, constraining the strength of SOTA claims.
- Hyperparameter sensitivity: choices such as number of scales (N=4), kernel sizes, attention configuration, and loss weight α=0.1 are empirical; their sensitivity and principled selection are not studied.
- Respiratory and cardiac coupling delays: potential subject-specific time delays between mechanical (radar) and electrical (ECG) signals are not modeled; whether time-warping or adaptive alignment improves reconstruction is untested.
- Safety and ethics: no discussion of clinical risk if reconstructed ECG is used for decision-making, nor regulatory considerations for medical deployment.
Glossary
- Adam optimizer: A stochastic gradient-based optimization algorithm commonly used to train neural networks. "Training is performed using the Adam optimizer for $1000$ epochs, with a batch size of $256$, and a learning rate of ."
- Adaptive neuro‑fuzzy network (ANFN): A hybrid model combining neural networks and fuzzy logic to capture nonlinear relationships. "Kim et al. \cite{neurofuzzy} designed an adaptive neuro fuzzy network (ANFN), that extracts features from the multilevel wavelet decomposition of radar signal for the ECG reconstruction."
- Approximation and detail components: The low-frequency (approximation) and high-frequency (detail) parts produced by wavelet decomposition. "the wavelet transform decomposes a signal using high-pass and low-pass filters to obtain detailed and approximate components, respectively."
- Bandpass/adaptive filtering: Signal processing techniques for isolating desired frequency bands or adapting to signal characteristics. "Respiration suppression was then applied using techniques such as bandpass/adaptive filtering, subspace methods, or wavelet decomposition."
- BioSPPy toolbox: A Python library for biosignal processing (e.g., ECG peak detection). "We use the BioSPPy toolbox \footnote[1]{Available online: \url{https://biosppy.readthedocs.io/en/stable/\#\%23welcome-to-biosppy} to detect the R-peaks in the ECG signal."
- Channel attention: A mechanism that weights feature channels to enhance informative ones. "Finally, we incorporate a channel-attention layer \cite{channel_attention}, to capture more distinctive information from the features along the channel dimension."
- Channel-shuffling: An operation that permutes feature channels to improve information mixing. "followed by channel-shuffling, where the feature channels are shuffled to promote information exchange among the aggregated features."
- Chest-wall displacement: Motion of the chest surface captured by radar as a proxy for cardiopulmonary activity. "derive the chest-wall displacement time-series signal following \cite{neonatal}"
- Clock drift: Gradual divergence between sampling clocks of different devices that requires compensation. "compensate for any clock drift, ensuring sub-sample alignment between the radar displacement signal and the reference ECG signal."
- Continuous-wave (CW) radar: A radar that transmits a constant-frequency signal to measure motion via phase changes. "a 24 GHz continuous-wave (CW) six-port radar system"
- Cross-correlation: A signal processing operation for measuring similarity and aligning signals in time. "utilizing a shared Gold code sequence and cross-correlation to precisely correct the time lag between the two systems."
- Cross-domain transformation: Mapping between different signal modalities (e.g., mechanical radar to electrical ECG). "radar-to-ECG reconstruction inherently requires a cross-domain transformation."
- CSConv layer: A convolutional module using multiple kernel sizes sequentially to capture multi-scale local features. "We adopt the CSConv layer \cite{latis}, where four convolution operations with different kernel sizes are applied sequentially."
- Demodulation: Processing to retrieve baseband information from modulated radar signals. "Early radar-based methods followed a signal processing pipeline beginning with radar I/Q extraction, demodulation, and phase unwrapping"
- Diffusion model: A generative model that iteratively denoises data to sample from complex distributions. "Air-ECG \cite{airecg} employed a diffusion model to better preserve ECG morphology."
- Discrete Fourier transform (DFT): A mathematical transform converting discrete signals into frequency components. "calculating the discrete Fourier transform (DFT) of each segment of windowed data."
- Doppler radar: Radar that measures frequency shifts due to motion, useful for cardiopulmonary monitoring. "Non-contact measurements were conducted using a 24.25 GHz Doppler radar unit with I/Q channels"
- Excitation–contraction coupling (ECC): The physiological mechanism linking electrical activation to mechanical contraction of the heart. "arising from the excitation–contraction coupling (ECC) mechanism \cite{cardiac_model}"
- Generative adversarial network (GAN): A framework of two competing neural networks used for generative modeling. "RS2ECG \cite{rfecg} leveraged a generative adversarial network (GAN) for radar-to-ECG mapping"
- Gated recurrent units (GRUs): A type of recurrent neural network cell designed for sequence modeling. "followed by CNN and gated recurrent units (GRUs) for feature extraction and ECG reconstruction."
- Gold code sequence: A set of pseudorandom sequences used for robust synchronization. "utilizing a shared Gold code sequence and cross-correlation to precisely correct the time lag between the two systems."
- Hanning window: A window function used in spectral analysis to reduce leakage. "we use Hanning window with three window lengths of $800$, $400$, and $200$, respectively."
- Harmonic summation: Combining harmonics in the frequency domain to enhance periodic signal detection. "heartbeats were tracked through spectral peaks, harmonic summation, or template matching"
- Heart Rate Variability (HRV): Variability in time intervals between heartbeats, a marker of autonomic regulation. "downstream vital sign estimation (Heart Rate (HR) and Heart Rate Variability (HRV))"
- Inverse lifting unit (ILU): The module that reconstructs signals from approximation and detail components in lifting wavelets. "The inverse lifting unit reconstructs the output signal feature from the input approximation and detail components"
- Inverse STFT: The operation that converts time-frequency STFT representations back to time-domain signals. "and subsequently applied inverse STFT to recover the final ECG signal."
- I/Q extraction: Obtaining in-phase and quadrature components from radar for displacement estimation. "Early radar-based methods followed a signal processing pipeline beginning with radar I/Q extraction, demodulation, and phase unwrapping"
- Layer normalization: A normalization technique applied across features within each layer to stabilize training. "First, layer normalization \cite{layerNorm} is applied to normalize the distribution of intermediate features"
- Lifting scheme: A method for constructing wavelets using predict and update steps, enabling custom, learnable transforms. "Sweldens \cite{1995lifting} introduced the lifting scheme, a custom-designed method for constructing wavelets."
- Lifting wavelet network: A neural architecture built using lifting-based wavelet operations. "We present LifWavNet, a lifting wavelet network based on a multi-resolution analysis and synthesis (MRAS) model for radar-to-ECG reconstruction."
- Mean absolute error (MAE): The average absolute difference between estimated and reference values. "We compare the estimated HR and RMSSD from the reconstructed ECG with those from the ground truth ECG using the mean absolute error (MAE)."
- Mean relative error (MRE): The average absolute error normalized by the magnitude of the reference signal. "We use the Pearson correlation coefficient () and the mean relative error (MRE) to evaluate the accuracy of the reconstructed ECG against the ground truth signal ."
- Mother wavelets: Prototype wavelets from which a family of wavelets is derived. "The choice of mother wavelets in the filter banks is typically guided by their similarity to the characteristics of the target signal \cite{ecgwavelet}."
- Multi-head self attention: An attention mechanism that computes several parallel attention heads to capture dependencies. "followed by a multi-head self attention operation."
- Multi-resolution analysis (MRA): Decomposition of a signal into multiple scales using wavelets. "the radar signal is decomposed into approximation and detail components through multi‑resolution analysis (MRA)"
- Multi-resolution analysis and synthesis (MRAS): A framework that decomposes and then recombines signal components across scales. "a multi-resolution analysis and synthesis (MRAS) model for radar-to-ECG reconstruction."
- Multi-resolution STFT loss: A loss combining STFTs with different window sizes to balance time-frequency resolutions. "we propose a multi‑resolution STFT loss to constrain the reconstructed ECG against ground truth in both the temporal and spectral domains."
- Multi-resolution synthesis (MRS): The recombination stage that reconstructs signals from multi-scale components. "then these components are recombined via multi‑resolution synthesis (MRS) to generate ECG waveforms."
- Multitask learning (MTL): Training a model to optimize multiple related tasks simultaneously. "later extended it to RadarODE-MTL \cite{radarodemtl}, which incorporated multitask learning (MTL)."
- Ordinary differential equation (ODE)-embedded network: A neural network integrating ODE formulations to model dynamics. "Zhang et al. \cite{radarode} developed RadarODE, an ordinary differential equation (ODE)-embedded network for ECG reconstruction"
- Photoplethysmography (PPG): An optical technique that measures blood volume changes in tissue. "Advancements in optical photoplethysmography (PPG) have introduced wearable devices that offer a less obtrusive option"
- Predict and update steps: The two core operations in the lifting scheme to derive detail and approximation signals. "the high-pass and low-pass filters are implemented via predict and update steps."
- QRS complex: The prominent ECG depolarization waveform associated with ventricular contraction. "isolate sharp transients such as QRS complexes while preserving low frequency morphology (P/T waves and baseline)"
- Random body movement (RBM): Motion artifacts from spontaneous subject movement that degrade signal quality. "to ensure a good signal-to-noise ratio (SNR) with minimal random body movement (RBM) noise."
- Remote PPG (rPPG): Contact-free PPG obtained from video imaging of skin color changes. "Remote PPG (rPPG) enables contact-free monitoring using visual cameras"
- Resampling factor: A scaling parameter used to adjust sampling rates for alignment. "an optimization routine determined an exact resampling factor to compensate for any clock drift"
- Root mean square of successive differences (RMSSD): An HRV metric computed from successive RR interval differences. "Then, in order to estimate the HRV parameter, we calculate the root mean square of successive differences (RMSSD), defined as:"
- Short-time Fourier transform (STFT): A time-frequency analysis technique using windowed Fourier transforms. "The STFT analyzes how the frequency content of a non-stationary signal changes over time."
- Signal-to-noise ratio (SNR): A measure of signal quality relative to background noise. "to ensure a good signal-to-noise ratio (SNR) with minimal random body movement (RBM) noise."
- Six-port radar: A radar front-end configuration with six ports enabling quadrature demodulation. "a 24 GHz continuous-wave (CW) six-port radar system"
- Strided convolution: A convolution operation with stride greater than one for downsampling. "we first use a strided convolution to downsample the signal to ."
- Strided deconvolution: A transposed convolution used for upsampling features. "Then we apply a strided deconvolution to upsample and produce the reconstructed feature ."
- Subspace methods: Signal processing techniques that decompose data into signal and noise subspaces. "Respiration suppression was then applied using techniques such as bandpass/adaptive filtering, subspace methods, or wavelet decomposition."
- Sym4 wavelet: A specific member of the Symlet wavelet family used in ECG processing. "WaveGRUNet, which applies Sym4 wavelet-based multilevel decomposition to radar signals"
- Task Force Monitor (TFM): A medical-grade device for recording reference ECG and other vitals. "The ground-truth electrocardiogram (ECG) was recorded using a medical-grade Task Force Monitor (TFM)."
- Template matching: A technique for detecting patterns by correlating with predefined templates. "heartbeats were tracked through spectral peaks, harmonic summation, or template matching"
- Tilt table: A clinical apparatus that positions subjects at controlled angles during monitoring. "During the experiments, subjects were positioned on a tilt table"
- Transformer attention: Mechanism in transformer models capturing long-range dependencies via self-attention. "applied transformer attention to capture long-range dependencies in ECG signals"
- U‑Net: An encoder–decoder neural architecture with skip connections, commonly used for reconstruction tasks. "RadarNet \cite{radarnet} presented a U-Net–based architecture with an FFT-based loss function"
- WaveGRUNet: A prior model combining fixed wavelet decomposition with CNN/GRU for ECG reconstruction. "Xu et al. \cite{wavegru} proposed WaveGRUNet, which applies Sym4 wavelet-based multilevel decomposition to radar signals"
- Wavelet transform: A time-frequency transform providing localized, multi-scale signal analysis. "Wavelet transform enables signal analysis across multiple frequencies with varying time resolutions and has demonstrated strong performance in both signal and image processing domains"
Practical Applications
Immediate Applications
Below is a concise set of actionable use cases that can be deployed now, leveraging LifWavNet’s learnable lifting-wavelet MRAS framework and multi-resolution STFT loss for radar-to-ECG reconstruction. Each bullet highlights sector, potential tools/products/workflows, and feasibility assumptions.
- Healthcare (clinical monitoring at rest)
- Use case: Contactless heart rate (HR) and heart rate variability (HRV) monitoring for patients who are resting or minimally moving (e.g., isolation wards, sleep labs, burn care, dermatology, fragile skin patients, elderly).
- Tools/products/workflows:
- “ECG-from-Radar Bedside Module”: 24/60 GHz radar unit mounted 15–40 cm from chest + edge device running LifWavNet + R-peak detection (e.g., BioSPPy) + dashboard for HR/HRV trends.
- Workflow: Radar I/Q → chest displacement extraction → LifWavNet inference → HR/HRV analytics → integration with hospital monitoring systems.
- Assumptions/dependencies: Minimal motion; line-of-sight; radar placement close to chest; current performance suited for HR/HRV trend tracking rather than diagnostic-grade ECG; requires local RF compliance and clinical validation per site.
- Telemedicine and home wellness
- Use case: Contactless sleep and daily wellness tracking (HR/HRV) using smart speakers or wall-mounted devices with mmWave radar (e.g., Google Soli-class modules).
- Tools/products/workflows:
- Consumer app + “Home ECG-from-Radar” device; automated nightly sessions; HR/HRV summaries and alerts for abnormal trends.
- Assumptions/dependencies: Stable positioning during sleep; privacy permissions; cloud/edge compute for inference; not a medical-grade diagnostic.
- Automotive (driver monitoring)
- Use case: In-cabin radar to estimate driver HR/HRV for fatigue/stress monitoring; combine with camera and steering behavior.
- Tools/products/workflows:
- “Cabin Vital Monitor”: Headliner radar + LifWavNet on automotive ECU; basic alerts for elevated stress or fatigue.
- Assumptions/dependencies: Moderate motion tolerance; effects of clothing/seatbelts; requires validation across seats and driving conditions; limited to trends rather than diagnostics.
- Workplace wellness and IoT
- Use case: Smart chair/desk radar monitoring employee HRV to track stress during sedentary work.
- Tools/products/workflows:
- “Desk Vital Plugin”: Small radar module + LifWavNet microservice + HRV dashboard and periodic reports.
- Assumptions/dependencies: Employee consent and privacy; stationary periods; non-diagnostic use; workplace policy compliance.
- Academia (research and teaching)
- Use case: A reproducible baseline for cross-domain physiological signal reconstruction; benchmarking on CR-RVS and Med-Radar datasets; curriculum modules in signal processing and machine learning.
- Tools/products/workflows:
- Implement LifWavNet and MR-STFT loss in standard frameworks; use as a teaching asset for multi-resolution cross-modal mappings; open research on model interpretability via feature visualizations.
- Assumptions/dependencies: Access to public datasets; adherence to reported pre-processing (I/Q demodulation, displacement extraction, resampling).
- Software and vendor SDKs
- Use case: Radar vendors and integrators providing an inference SDK for contactless HR/HRV.
- Tools/products/workflows:
- “LifWavNet Inference SDK”: API that takes displacement signals and outputs ECG estimates + HR/HRV; plugins for BioSPPy; containerized microservice for edge gateways.
- Assumptions/dependencies: Stable chest displacement extraction pipeline; windowed inference (e.g., 5.12 s segments); on-device acceleration optional (quantization/pruning if needed).
Long-Term Applications
The following applications require further research, scaling, robustness improvements, clinical trials, and/or regulatory clearance before broad deployment.
- Healthcare diagnostics (clinical-grade ECG from radar)
- Use case: Continuous diagnostic ECG (PQRST morphology fidelity) for arrhythmia detection (AFib, PVCs), ischemia monitoring, and in-ICU cardiac surveillance without electrodes.
- Tools/products/workflows:
- “Contactless Clinical ECG Device”: Bedside radar array + LifWavNet v2 with motion robustness + hospital-grade analytics; integration with EHR and alarm systems.
- Assumptions/dependencies: Large-scale clinical trials; rigorous validation in diverse populations/postures; motion robustness; regulatory approvals (e.g., FDA/CE); clear performance under clothing and blankets.
- Neonatal and fetal monitoring
- Use case: NICU monitoring of fragile infants; contactless fetal ECG through maternal abdomen (research-grade initially).
- Tools/products/workflows:
- Specialized radar placement and safety protocols; personalized model adaptation; motion suppression strategies; clinical study workflows.
- Assumptions/dependencies: Sensitivity to very small motion; maternal-fetal signal separation; safety, ethics, and regulatory compliance.
- Emergency response and triage
- Use case: Rapid contactless vitals acquisition in disaster zones, pandemics, or hazardous environments; through PPE or light clothing.
- Tools/products/workflows:
- Portable radar kits + real-time LifWavNet inference; triage dashboard for HR/HRV and basic ECG morphology cues.
- Assumptions/dependencies: Robustness to clutter, occlusion, multiple subjects; battery-powered edge compute; field validation.
- Public health screening in high-traffic spaces
- Use case: Airports, clinics, and public buildings monitoring basic cardiac metrics unobtrusively for early risk screening.
- Tools/products/workflows:
- Multi-radar installations; anonymized aggregate analytics; alerting policies for critical anomalies.
- Assumptions/dependencies: Strong privacy protections; opt-in frameworks; high specificity to avoid false alarms; policy and ethical guidelines.
- Robotics and eldercare
- Use case: Service robots that continuously monitor vital signs of patients/residents; fall detection + cardiac trend monitoring.
- Tools/products/workflows:
- Robot-mounted radar arrays + sensor fusion (rPPG, thermal, IMU) + adaptive LifWavNet; workflows for remote caregiver dashboards.
- Assumptions/dependencies: Multi-person disambiguation; navigation and placement constraints; long-term autonomy and safety standards.
- Multimodal sensor fusion and personalization
- Use case: Combining radar with rPPG, thermal cameras, and microphones to improve robustness; personalized LifWavNet adapting to body habitus and posture.
- Tools/products/workflows:
- Federated learning pipelines; on-device personalization; unified biosignal fusion architectures; adaptive MR-STFT regimes.
- Assumptions/dependencies: Data governance for federated learning; calibration-free deployment; diverse training datasets.
- Edge optimization and hardware acceleration
- Use case: Real-time on-device inference on low-power microcontrollers or radar SoCs (e.g., TI IWR, NXP TEF).
- Tools/products/workflows:
- Model compression (pruning/quantization); DSP/NN accelerator kernels; co-design with radar firmware for synchronized windows.
- Assumptions/dependencies: Maintaining signal fidelity under compression; deterministic latency; co-optimization with chest displacement extraction.
- Standards, regulation, and reimbursement
- Use case: Establishing clinical standards for radar-based ECG, measurement protocols, and reimbursement codes.
- Tools/products/workflows:
- Policy frameworks defining acceptable use, accuracy benchmarks, validation protocols, and privacy; industry consortia and clinical societies drafting guidance.
- Assumptions/dependencies: Multi-center trials; consensus on metrics beyond HR/HRV (e.g., morphology fidelity indices); alignment with medical device regulations and data protection laws.
- Insurance and occupational health
- Use case: Long-term risk assessment via contactless vitals trends (e.g., life and health insurance, occupational screening).
- Tools/products/workflows:
- Secure analytics platforms; opt-in employee/member programs; risk-adjusted models informed by HRV and cardiac trends.
- Assumptions/dependencies: Ethical use, transparency, and consent; strict privacy controls; avoidance of bias and misuse.
- Academic extensions to other cross-domain signals
- Use case: Applying lifting-wavelet MRAS with multi-resolution losses to other cross-domain mappings (e.g., radar-to-respiration morphology, seismic-to-structural health signals).
- Tools/products/workflows:
- Open benchmarks; interpretability studies; curriculum modules on wavelet lifting in cross-domain reconstruction.
- Assumptions/dependencies: Access to paired datasets; tailoring MR-STFT windows to each modality; domain-specific validation protocols.
Collections
Sign up for free to add this paper to one or more collections.