Modified Rankin Scale (mRS) in Stroke Research
- Modified Rankin Scale (mRS) is an ordinal scale ranging from 0 to 6 that quantifies post-stroke disability and functional independence.
- Recent approaches integrate tractographic features, capturing both focal lesion metrics and brain network disruptions for enhanced outcome prediction.
- Predictive models using techniques like Random Forest regression and recursive feature elimination outperform traditional volumetric methods in mRS assessment.
The modified Rankin Scale (mRS) is the principal clinical outcome measure utilized in stroke research and trials to assess post-stroke disability. Quantified as an integer score ranging from 0 (no symptoms) to 6 (death), mRS encapsulates a subject's overall functional independence. Its widespread adoption as an endpoint in cerebrovascular research stems from its capacity to summarize diverse neurologic deficits and daily life impact in a single ordinal scale. Notably, in contemporary predictive modeling, mRS prediction has advanced from first-order lesion metrics to functionally motivated features that incorporate brain-wide connectomic disruptions (Kao et al., 2019).
1. Definition and Clinical Relevance
The mRS is an ordinal scale with grades 0–6, where:
- 0: No symptoms
- 1: No significant disability despite symptoms
- 2: Slight disability
- 3: Moderate disability
- 4: Moderately severe disability
- 5: Severe disability
- 6: Death
It is the standard for reporting outcomes at 3 months post-stroke in clinical trials and observational cohorts. The scale condenses complex neurologic and functional status into a tractable measure for both clinical and algorithmic analysis. In predictive research, the mRS serves as the ground truth label for outcome modeling tasks (Kao et al., 2019).
2. Conventional Feature Sets and Limitations
Historically, first-order lesion features have been the most prevalent inputs for mRS prediction:
- Volumetric features: total lesion volume (1D)
- Spatial features: lesion centroid coordinates (3D)
- Morphological features: axes length, ratio, solidity, roundness, surface (6D)
- Volumetric‐spatial features: lesion volume per AAL region (116D)
These features, though widely used, primarily measure structural or geometric aspects of the lesion without accounting for disruptions extending beyond the focal damage. The gold standard has been the lesion volume, which models direct tissue damage but may underestimate remote neural consequences mediated via disrupted brain networks (Kao et al., 2019).
3. Tractographic Feature Construction
Recent approaches emphasize the importance of second-order lesion effects—namely, the predicted disconnection of remote, functionally significant regions due to the stroke. Kao et al. (2019) introduced the tractographic feature, computed as follows:
- Average Connectome Formation From 1,021 Human Connectome Project subjects, individual tractograms are constructed using q-space diffeomorphic reconstruction and deterministic tractography (DSI Studio), with brain parcellation into regions (AAL atlas). Connectivity count matrices are retained for each healthy subject.
- Disruption Matrix () For a patient lesion (MNI space), seeds are placed in every voxel; streamlines are tracked (using average ODFs) and a disruption matrix , enumerating streamlines connecting regions and that transit the lesion, is built.
- Normalization and Impact Quantification is normalized by its maximal entry , yielding . Raw disruption scores for each region are the column sums . The lesion-region volume weighting vector (where is volume of inside region ) is formed.
- Feature Vector Final tractographic feature: After Z-normalization and variance filtering, recursive feature elimination selects the top AAL regions most predictive of mRS.
4. Predictive Modeling Protocols
Kao et al. (2019) structured mRS outcome prediction as a regression-and-rounding problem. A Random Forest Regressor (300 trees, depth 3) minimizes mean absolute error (MAE) on the training set:
where is the ground-truth mRS. At inference, predictions are rounded:
Evaluation is performed using leave-one-out cross-validation (LOOCV) on 37 subjects from the ISLES 2017 dataset. Performance is assessed by classification accuracy and mean absolute error (AE):
- Accuracy:
- AE:
5. Comparative Results and Quantitative Insights
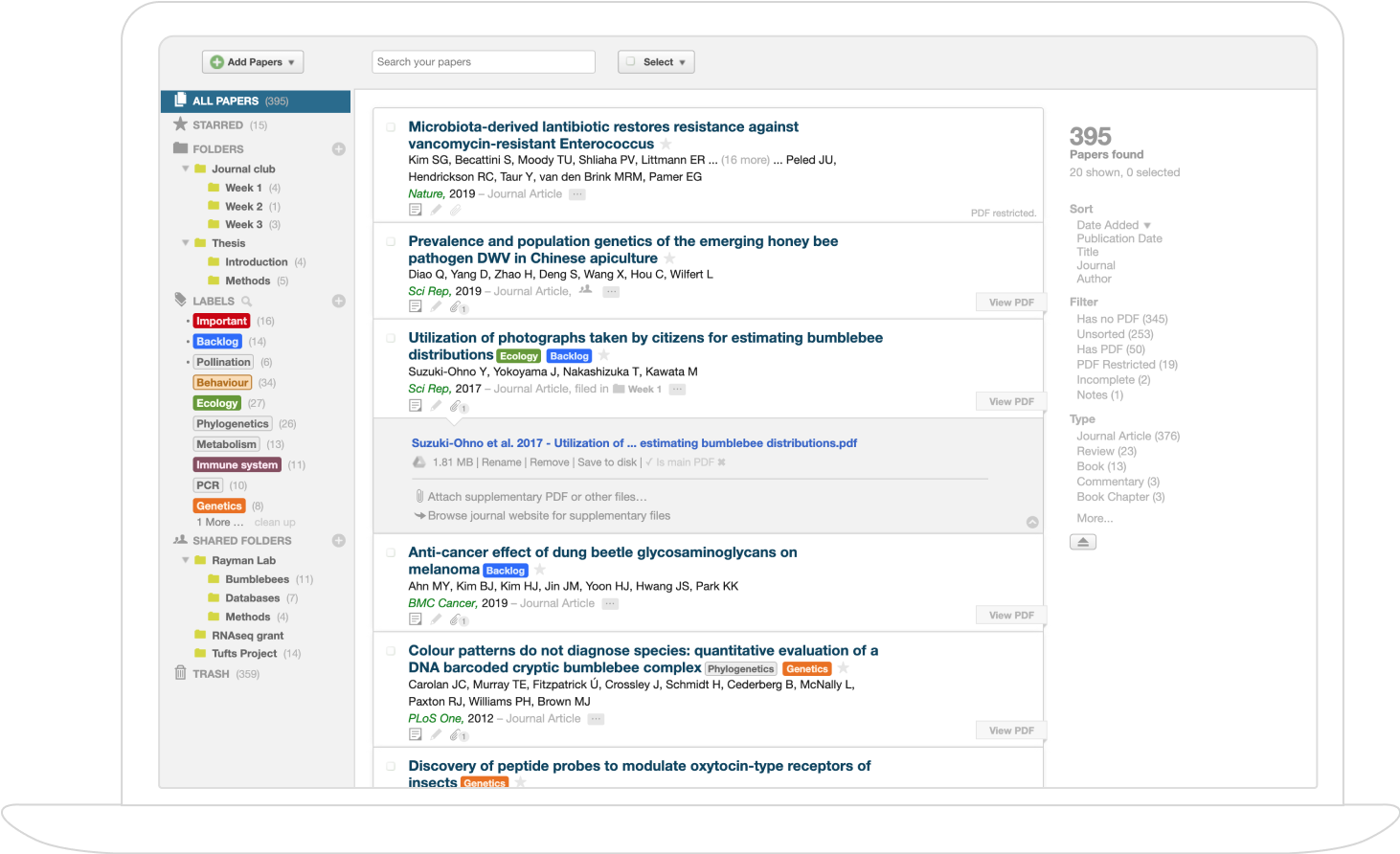
A summary of mRS prediction performance across feature types is provided below:
| Feature Type | Accuracy | Avg. Abs. Error (mean ± std) |
|---|---|---|
| Tractographic (116D→8D after RFECV) | 0.622 | 0.487 ± 0.683 |
| Volumetric (1D) | 0.514 | 0.595 ± 0.715 |
| Volumetric-spatial (116D) | 0.568 | 0.621 ± 0.817 |
| Morphological (6D) | 0.378 | 0.703 ± 0.609 |
| Spatial (3D) | 0.351 | 0.919 ± 0.882 |
| Maier & Handels (1,662D) | 0.595 | 0.460 ± 0.597 |
The tractographic feature yields the highest overall accuracy (62.2%) and a low mean absolute error (0.487), surpassing all first-order lesion-based baselines and marginally improving upon the state-of-the-art Maier & Handels feature set in accuracy. The tractographic approach generalizes better despite lower dimensionality, indicating that anatomically motivated connectivity disruptions are more informative for post-stroke disability estimation than raw image-derived feature sets (Kao et al., 2019).
6. Methodological Implications and Functional Interpretation
The core insight is that tractographic features encode second-order lesion effects: by tracking the predicted disconnection of remote, functionally relevant brain regions, these features reconcile local tissue damage with systemic neural consequences. Recursive feature elimination highlights eight AAL regions, with weighted disruption in the left inferior temporal gyrus showing maximum predictive value—potentially due to its role in language function and inter-hemispheric tracts.
A plausible implication is that mRS scores derive not merely from lesion size or shape, but from the global reconfiguration of connectivity networks precipitated by the lesion. The hybrid regression-to-classification scheme enables continuous MAE optimization while producing discrete mRS grades, providing robustness over conventional regression or multiclass classification approaches.
7. Current Directions and Limitations
Recent work underscores the necessity of integrating connectomic information into outcome prediction workflows. While tractographic features demonstrate improved accuracy, per-grade mRS performance remains undelineated in available studies. The reliance on population-average connectomes and deterministic tractography, as opposed to patient-specific networks, presents a methodological limitation. Ongoing research may explore individualized connectomic models, advanced feature selection protocols, and prospective clinical validation to further refine mRS prediction paradigms.
In summary, the mRS is the dominant post-stroke disability outcome metric. Its predictive modeling has advanced towards functionally grounded, tractography-based features that encapsulate both focal damage and wider brain network disruptions, yielding superior prognostic accuracy over prior volumetric and morphological benchmark methods (Kao et al., 2019).