Decision Curve Analysis Overview
- Decision Curve Analysis is a method that quantifies the net benefit of predictive models by integrating threshold-dependent trade-offs between true and false positives.
- DCA employs mathematical formulations, including Bayesian methods, to assess uncertainty and optimize decision strategies based on cost-benefit structures.
- Extensions of DCA, such as multi-treatment frameworks and integration with cost curves and Brier scores, enhance model evaluation in clinical and machine learning contexts.
Decision curve analysis (DCA) is a model evaluation methodology that quantifies the clinical or practical utility of predictive models or decision strategies as a function of the decision threshold. It is widely used to assess features such as net benefit, threshold-dependent trade-offs, and decision relevance across diverse operating contexts. DCA is integral to evidence-based medicine, risk prediction, and increasingly to machine learning model evaluation, especially where calibrated probabilities serve as decision support.
1. Foundations and Scope of Decision Curve Analysis
DCA evaluates the consequences of model-based or rule-based classification by integrating outcome prevalence, the trade-off between true and false positives, and user-specified misclassification costs. Unlike conventional accuracy-focused metrics, DCA anchors evaluation in the expected utility (or clinical net benefit) for a range of thresholds, reflecting the underlying cost-benefit structure encountered in real-world decision-making. In standard medical use, the threshold is the minimum predicted risk at which intervention is justified, representing a patient’s (or decision-maker’s) preference or the relative utility of correct versus incorrect classifications. The methodology generalizes to decision support systems wherever threshold-based binary (or multiway) actions are taken.
2. Mathematical Formulation and Net Benefit
The net benefit (NB) at a given threshold is defined as: where and are the number of true and false positives at threshold , and is the total sample size. This formula directly encodes the relative utility of true positives to false positives, with reflecting the implied utility (or equivalently, cost ratio) at the decision threshold. When generalized to accommodate varying costs and multi-treatment settings, the net benefit incorporates per-strategy loss terms and, in more advanced extensions, risk differences and treatment-specific thresholds (Chalkou et al., 2022).
A Bayesian formulation samples from the posterior distributions of prevalence, sensitivity, and specificity, and propagates uncertainty throughout the net benefit calculation: where and are sensitivity and specificity at , and is prevalence (Cruz et al., 2023).
3. Extensions: Multiple Treatments and Meta-Analysis Integration
Traditional DCA treats binary interventions (“treat” vs. “do not treat”). Extensions support personalized treatment choices among multiple options using thresholds and risk difference calculations: denotes predicted risk difference for subject under treatment . These frameworks draw upon network meta-analysis (NMA) to pool evidence from multiple randomized controlled trials, allowing the estimation of treatment-specific event rates and appropriate population-level or individualized net benefit estimations (Chalkou et al., 2022). This generalization is particularly relevant for diseases with multiple competing therapies and heterogenous treatment effects.
4. DCA, Cost Curves, Brier Score, and Model Calibration
DCA is closely related to cost curves and the Brier curve in the decision-theoretic framework. The Brier score, which measures mean squared error between predicted probabilities and true outcomes, can be interpreted as averaging regret (cost-penalty) over a mixture of thresholds. For properly calibrated models, the area above the Decision Curve is equivalent to a (possibly bounded) Brier Score on the relevant threshold interval (Flores et al., 6 Apr 2025).
A key formula linking net benefit and Brier loss (Brier curve) at a threshold is: where is class prevalence and is the Brier loss at (Millard et al., 29 Sep 2025). At any , both net benefit and Brier loss will select the same model as optimal. However, differences in net benefit across thresholds are not commensurable, while Brier loss is consistently comparable across thresholds—a key distinction for evaluation over broad operating contexts.
The concept of the upper envelope decision curve defines the maximum achievable net benefit with perfect calibration at each threshold. The calibration gap—the difference between a model’s actual decision curve and this envelope—quantifies gains possible through recalibration.
| Method | Evaluates | Aggregates over |
|---|---|---|
| DCA | Net Benefit | Decision threshold |
| Brier Curve | Brier Loss | Cost/threshold proportion |
| Cost Curve | Expected Loss | Misclassification cost |
5. Bayesian and Statistical Uncertainty in DCA
Bayesian DCA models provide full posterior distributions for net benefit, allowing rigorous uncertainty quantification. Key probabilities include , the probability that a model surpasses standard-of-care strategies, and , the probability of being the optimal decision strategy among all candidates. Bayesian computation is often tractable in the binary case due to Beta-Bernoulli conjugacy, and extensions to survival data employ MCMC with Weibull likelihoods (Cruz et al., 2023).
Expected Value of Perfect Information (EVPI) quantifies the expected net benefit loss attributable to current epistemic uncertainty. This facilitates risk-averse policy decisions, motivating data acquisition or restraining practice shifts when evidence is equivocal.
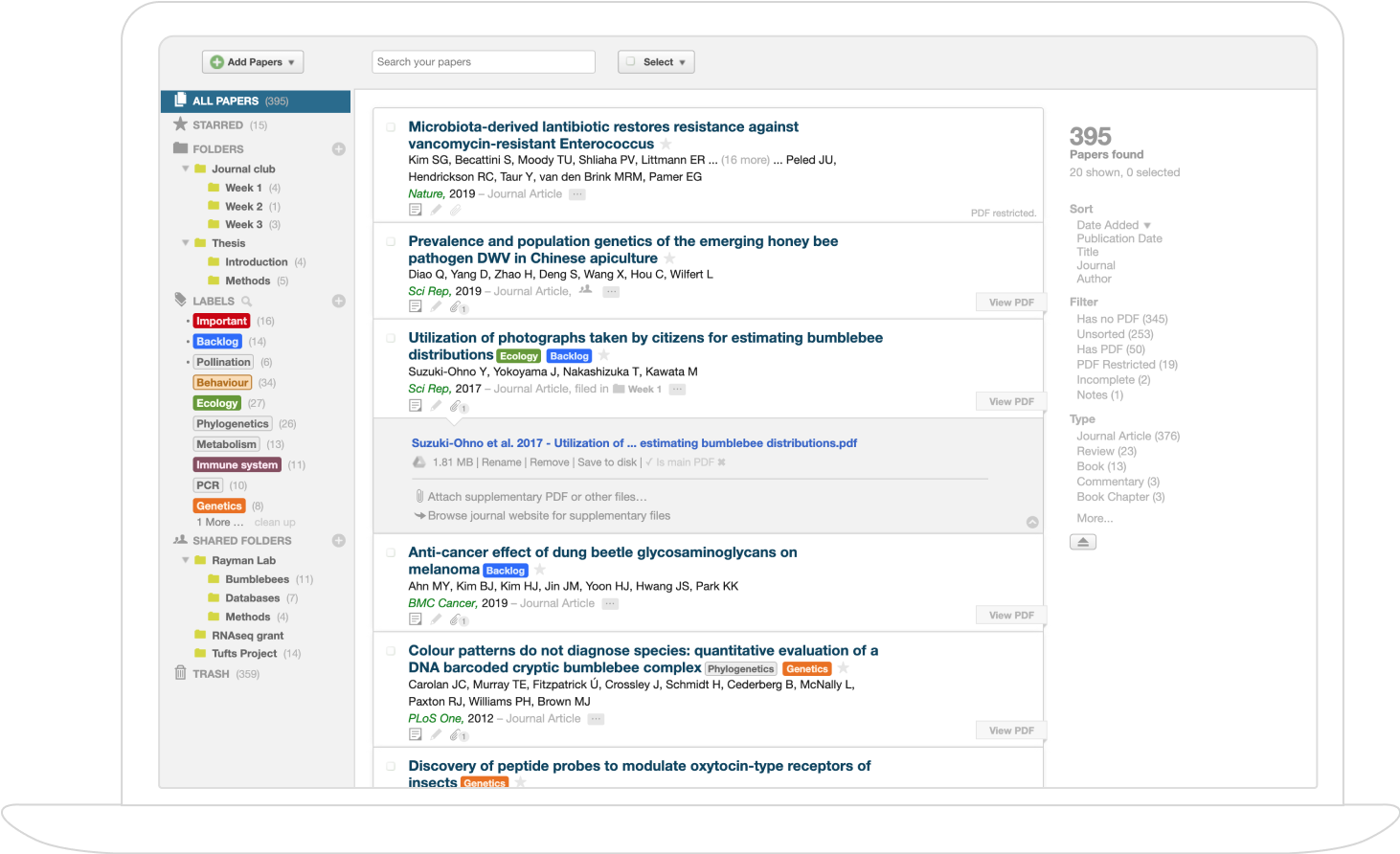
6. DCA in Machine Learning and Nonclinical Applications
Though most prominent in clinical epidemiology, DCA principles generalize to various domains involving probabilistic forecasting and threshold-based classification. In binary classification, DCA enables evaluation with respect to threshold uncertainty, offering a natural alternative to fixed-threshold metrics or threshold-agnostic measures such as AUC-ROC (Flores et al., 6 Apr 2025). The methodology directly addresses the disconnect between conventional evaluation—often based on single or average thresholds—and real-world decision policies, where cost trade-offs, prevalence, and user utility are rarely fixed.
Empirical studies demonstrate that machine learning literature, especially outside healthcare, underutilizes threshold-mixed (proper scoring rule-based) metrics, despite their superior alignment with consequentialist decision support (Flores et al., 6 Apr 2025). Python packages such as briertools and R packages such as bayesDCA are now available to support threshold-aware analysis and visualization.
7. Limitations, Calibration, and Future Directions
DCA requires well-calibrated probabilistic predictions; improper calibration can bias net benefit estimations and misinform downstream decisions. Reference lines (“treat all,” “treat none,” upper envelope) in DCA plots contextualize model performance relative to default or optimally recalibrated strategies. When operating context or cost structure is uncertain or variable, DCA provides a flexible summary, but care is needed interpreting net benefit differences across thresholds. Current research is focused on extending methodology to small or sparse congruent datasets, integrating richer patient or decision-maker utilities, handling multiple outcomes, and establishing robust measures of uncertainty that inform the expected value of further information (Chalkou et al., 2022, Cruz et al., 2023).
In summary, decision curve analysis is a principled and adaptable methodology for model evaluation where threshold-dependent utility is paramount. Its connection to proper scoring rules and cost curves grounds its use in decision theory, and Bayesian extensions advance its ability to handle epistemic uncertainty in risk-averse or high-stakes settings.