Classification-Based Clinician Availability
- The paper introduces a classification-based framework that integrates hierarchical Bayesian models and ILP scheduling to predict clinician availability with improved operational efficiency.
- It leverages both structured institutional data and unstructured free-text notes processed by LLMs to refine predictions, ensuring fairness and compliance with contractual constraints.
- Empirical validation demonstrates that the approach balances workload, reduces last-minute scheduling disruptions, and enhances clinician well-being through precise, data-driven scheduling solutions.
Classification-based clinician availability prediction refers to the use of supervised learning techniques, probabilistic modeling, and combinatorial optimization, often in conjunction with mathematical programming, to forecast the periods during which clinicians are available to provide care, and to inform subsequent scheduling or workload-balancing algorithms. Recent developments emphasize integrating structured institutional data and unstructured scheduling notes—leveraged via LLMs—into flexible predict-then-optimize (PTO) workflows. These approaches seek to maximize operational efficiency, ensure compliance with contractual obligations, promote equity, and improve clinician well-being in complex healthcare systems spanning multiple sites, teams, and levels of care.
1. Conceptual Overview and Historical Foundations
Classification-based clinician availability prediction is rooted in efforts to balance healthcare supply and demand, addressing the fundamental operational issue of aligning provider time (supply) with predicted clinical workload (demand). Early work focused on workload prediction using hierarchical models to account for multilevel sources of variability—at patient, team, and facility granularity—enabling partition of variance and direct comparison of predicted demand against fixed provider supply vectors, as exemplified in Department of Veteran Affairs PCMH studies (Shams et al., 2014). The evolution toward predictive classification reflects the granularity and immediacy required for modern scheduling, where operational realities demand not only workload forecasts but granular, per-shift or per-day predictions of individual clinician availability.
2. Hierarchical and Multivariate Modeling for Availability Forecasts
A foundational approach utilizes multivariate hierarchical Bayesian frameworks to jointly model multiple response outcomes pertinent to clinical workload, such as primary and non-primary care relative value units (RVUs) (Shams et al., 2014). Let denote the workload for outcome (e.g., primary or non-primary care) for patient , assigned to team at facility . The modeling structure consists of:
- Patient level: where are coefficients for patient-level covariates (demographic, diagnostic, utilization).
- Team level: incorporating team-level covariates and random effects .
- Facility level: with facility-level predictors and corresponding random effects.
This multilevel structure facilitates decomposition of variance, quantification of clustering, and adjustment for unobserved heterogeneity. Applied to clinician availability, the predicted workload distribution is used to compare with deterministic provider supply vectors (hours available), evaluating the match between anticipated demand and real-world availability constraints.
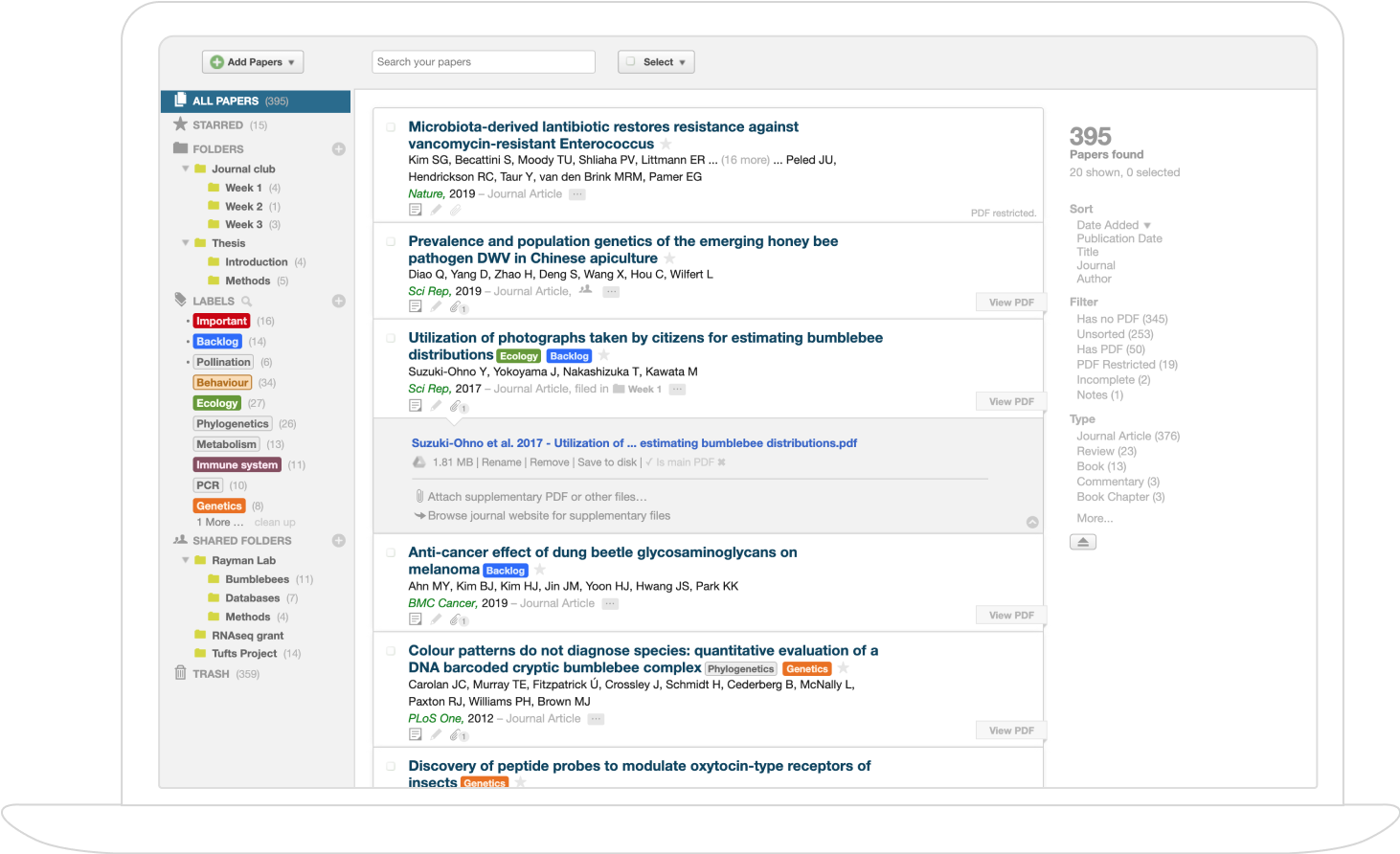
3. Mathematical Optimization for Clinician Scheduling
Integer linear programming (ILP) formulations are a mainstay for the translation of clinician availability predictions into actionable schedules (Landsman et al., 2019, Jha et al., 2 Oct 2025). Central to these models are assignment variables, coverage, fairness, and preference constraints, as outlined in Table 1.
| Construct | Variable / Constraint | Description |
|---|---|---|
| Assignment | , , | Binary indicators: clinician to block /service ; weekend ; shift on day |
| Minimum/Maximum | Required number of blocks/services for clinician | |
| Equity | Equal distribution of weekends/holidays | |
| Preferences | Time-off requests for blocks and weekends |
Hard constraints guarantee demand coverage (each block/weekend is filled) and prohibit overwork (no consecutive undesirable assignments). Soft objectives include accommodation of clinician preferences and maximizing block-weekend adjacency, operationalized via weighted normalized penalty terms and auxiliary variables for linearization (Landsman et al., 2019).
4. LLM-Enhanced Predict-then-Optimize (PTO) Paradigm
Recent advances extend traditional ILP scheduling pipelines by integrating predictive models for clinician availability enhanced with LLMs (Jha et al., 2 Oct 2025). The PTO paradigm comprises:
- Classification-Based Prediction: Structured features (historical data, temporal context) are input into classifiers (commonly logistic regression, but also possible with tree-based models), producing (Equation 4). LLMs (e.g., FLAN-T5) process free-text schedule notes, extracting binary constraints . The final probability is hard-set to zero for explicit conflicts:
(Equation 5).
- MIP-Based Scheduling:
The refined inform the feasible assignment set and appear as weights in the objective. Schedule optimization (Equation 2) maximizes a weighted sum of: - cFTE compliance (: deviation from target shifts), - workload equity (: fairness in shift distribution), - realized availability (: maximizing ), - schedule consistency with previous solutions ().
The LLM-augmented pipeline ensures that implicit, unstructured preferences and constraints—otherwise overlooked—are directly encoded into the scheduling optimization, reducing label noise and increasing compliance with qualitative inputs.
5. Empirical Validation and Findings
Large-scale empirical validation demonstrates the practical benefits of these integrated approaches:
- Variance Partitioning for Demand: In analyses of VA medical center data, 61% of primary care workload variation was attributable to patient-level effects, 17% to team, and 22% to facility; for non-primary care, 79% was patient, 5% team, 16% facility. This quantification enables targeted interventions (e.g., adjusting staffing at high-variance teams) (Shams et al., 2014).
- Scheduling Efficacy: ILP-generated clinician schedules strictly satisfy all hard constraints and provide superior accommodation of preferences (time-off, block-weekend adjacency) compared to manual schedules, with sensitivity analysis showing computational feasibility up to multi-year horizons (Landsman et al., 2019).
- LLM-Augmented Availability: Incorporation of LLM-derived signals directly into probabilistic availability predictions ensures that explicit free-text indications (e.g., "unavailable: conference") cannot be overridden by historical trends, resulting in schedules that are both operationally robust and sensitive to evolving individual constraints (Jha et al., 2 Oct 2025).
6. Impact on Healthcare Operations and Clinician Well-Being
The structured integration of classification-based predictions into schedule optimization leads to multifaceted operational improvements:
- Operational Efficiency: Schedules optimized with accurate availability predictions reduce last-minute disruptions, improve resource utilization, and guarantee coverage aligned with demand.
- Fairness and Equity: Balancing shift assignments and penalizing deviations from average shares mitigates workload imbalances, directly impacting morale and fairness perceptions.
- Well-Being and Job Satisfaction: Explicit modeling of availability and preferences—especially when extracted from unstructured data—promotes job satisfaction, reduces burnout, and increases retention, as schedules better reflect clinician-identified needs.
A plausible implication is that as LLMs continue to improve in the extraction of nuanced signals from unstructured clinician inputs, the granularity and quality of availability predictions—hence schedule acceptability and system resiliency—will further increase.
7. Extensions, Limitations, and Prospective Directions
Classification-based clinician availability prediction frameworks are highly adaptable:
- Longitudinal Modeling: Hierarchical models can be extended to handle time-series data, enabling dynamic forecasting of demand and supply (Shams et al., 2014).
- Generalization to Multiple Outcomes: Methods are not restricted to clinical care portfolios but can capture other service types or auxiliary roles.
- Sensitivity to Constraints: Computational demands increase with concurrency of services and stringent constraints; relaxing the most limiting constraints (e.g., "no consecutive blocks") yields substantial speed-ups without major loss in optimality (Landsman et al., 2019).
- Separation of Prediction and Optimization: The modular PTO structure permits independent refinement and validation of both prediction and optimization components, enhancing transparency and facilitating adaptation to new data types (e.g., different clinical departments or institutions) (Jha et al., 2 Oct 2025).
The incorporation of LLMs as constraint-extraction engines from free-text notes signals a shift toward richer integration of qualitative clinician input into quantitative schedule management.
Conclusion
Classification-based clinician availability prediction encompasses a spectrum of scalable, mathematically rigorous methodologies for forecasting and operationalizing the presence of clinical staff. Contemporary approaches unify hierarchical Bayesian modeling, supervised probabilistic classification, LLM-based extraction of unstructured preferences, and multi-objective mathematical programming. These advances enable the reliable balance of healthcare supply and demand, the enforcement of fair and consistent scheduling, and the capture of nuanced clinician preferences, collectively contributing to enhanced operational robustness and workforce well-being within modern healthcare delivery organizations (Shams et al., 2014, Landsman et al., 2019, Jha et al., 2 Oct 2025).