- The paper proposes a hybrid deep learning framework that combines a 3D U-Net and DenseNet-VGG classifier with attention mechanisms to automate glioma segmentation and grading.
- The segmentation model achieved a Dice coefficient of 98% on the BraTS2019 dataset, while the classifier attained 99.99% accuracy, outperforming conventional CNNs.
- Attention modules, including multi-head, spatial, and channel attention, enhance model interpretability and refine feature extraction for clinical decision support.
Hybrid Deep Learning for Glioma Segmentation and Grading in 3D MRI
Introduction
This paper presents a comprehensive 3D MRI-based pipeline for automated glioma segmentation and grading, proposing a hybrid deep learning architecture that leverages both U-Net for segmentation and a DenseNet-VGG dual-path classifier augmented with multi-head, spatial, and channel attention mechanisms. The work addresses critical limitations in current glioma grading approaches, including error-prone manual annotation, insufficient exploitation of 3D spatial context, and the lack of advanced attention-based interpretability. The framework is quantitatively validated on the BraTS2019 dataset, demonstrating significant gains in both segmentation and classification metrics relative to conventional CNN models and previously reported results.
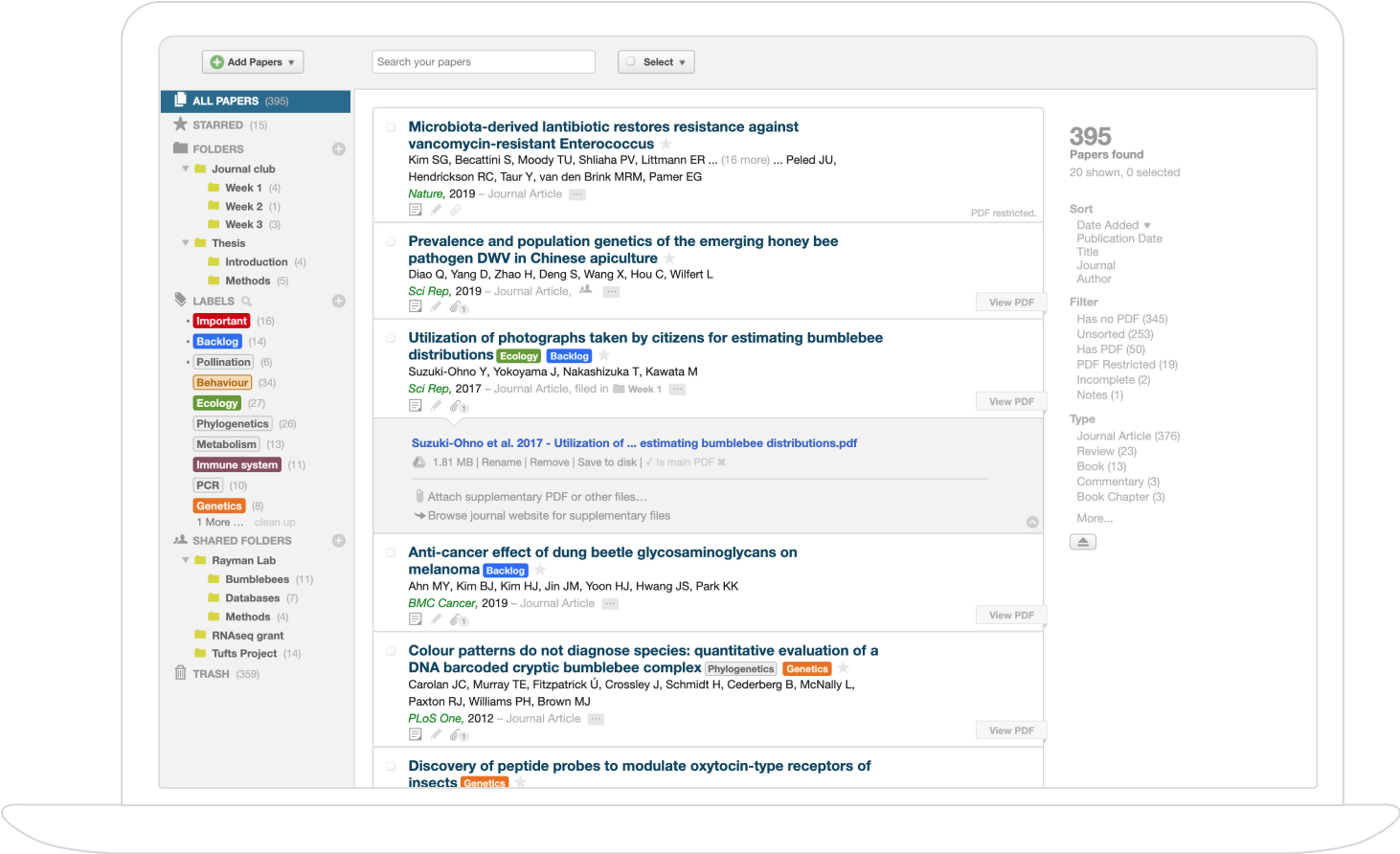
Methodology and System Architecture
The proposed methodology consists of a sequential five-step pipeline: dataset curation, robust preprocessing, tumor segmentation with a 3D U-Net backbone, feature extraction and classification via a hybrid DenseNet-VGG architecture with attention, and comprehensive evaluation using medical imaging benchmarks. Figure 1 illustrates the research methodology process, and Figure 2 depicts the system architecture in detail.

Figure 1: Research methodology pipeline outlining dataset curation, preprocessing, segmentation, hybrid classification, and evaluation.

Figure 2: Hybrid deep learning system integrating 3D U-Net for segmentation and DenseNet/VGG-based attention-augmented classifier.
The BraTS2019 dataset, comprising 335 annotated multi-modal MRI scans, is processed through a pipeline involving normalization, resampling to balance GPU constraints with diagnostic relevance, and advanced spatial/intensity augmentation, reducing overfitting risks and improving generalization. Manual ground-truth labels are binarized for robust tumor versus non-tumor discrimination.

Figure 3: Examples from the BraTS2019 3D MRI dataset highlighting raw input and expert segmentation.
3D U-Net Based Tumor Segmentation
The U-Net implementation operates natively in 3D, capturing volumetric contextual information. Its encoder-decoder structure, equipped with skip connections, ensures preservation of fine spatial details alongside comprehensive abstraction, enabling precise voxel-level boundary delineation that is essential in neuro-oncology.

Figure 4: 3D U-Net architecture processes volumetric MRI for demanding spatial localization tasks.
Enhancements are made through the introduction of soft additive attention gates: these spatially recalibrate the feature tensor such that the network’s capacity is preferentially allocated to tumor regions, suppressing background and improving precision in spatially ambiguous cases. This attention mechanism (Figure 5) is fully differentiable and supports end-to-end learning.

Figure 5: Attention gate modules enable spatial re-weighting and feature recalibration for both segmentation and classification.
The U-Net segmentation model achieves a Dice coefficient of 98% on validation, indicating near-perfect overlap between predicted and expert segmentations—exceeding typical clinical benchmarks for MRI tumor segmentation.
Hybrid DenseNet-VGG with Multi-Head, Spatial, and Channel Attention
Following segmentation, the pipeline forwards the localized tumor region to a novel, bifurcated DenseNet/VGG classifier, each with independent pathways. DenseNet facilitates deep feature reuse and mitigates vanishing gradients in very deep networks, while VGG’s depth and uniform architecture emphasize hierarchical abstraction across scales. The concatenated feature representation from both branches is passed through attention modules before classification.
Multi-head attention enables the network to simultaneously focus on orthogonal aspects of the tumor (e.g., morphology, margin heterogeneity, peritumoral edema), with spatial and channel attention further refining the feature importance map along clinically relevant dimensions. This provides both enhanced accuracy and interpretability; for example, certain heads may learn to discriminate microvascular proliferation or necrotic patterns distinctive of high-grade gliomas.

Figure 6: Categorical accuracy improvements across epochs with the multi-head attention-integrated classifier.
Quantitative Evaluation and Comparative Analysis
On the BraTS2019 validation partition (n=84), the proposed system attains a classification accuracy of 99.99%, F1-score of 0.99, and exceptionally high precision/recall, as demonstrated in the confusion matrix (Figure 7) and class-wise F1-score plot (Figure 8). These metrics significantly outperform all conventional CNN baselines (e.g., ResNet71, AlexNet, VGGNet), as shown in Figure 9.

Figure 8: F1-scores for HGG and LGG classes demonstrating balanced, robust performance.

Figure 7: Confusion matrix for the DenseNet-VGG hybrid classifier—nearly perfect discrimination between glioma grades.

Figure 10: Aggregate metrics (F1, accuracy, precision, recall) affirming overall classifier efficacy.

Figure 9: Bar graph comparison against state-of-the-art CNN architectures—proposed method leads in all key metrics.
The attention mechanism notably contributes to the improved performance, as ablation and comparison experiments reveal marked degradation when attention is omitted. The system’s segmentation and grading results set new benchmarks in the MRI-based brain tumor grading literature.
Discussion and Implications
From a clinical perspective, the proposed architecture's performance indicates strong readiness for deployment as a point-of-care decision support tool in neuroradiology. The architecture’s capacity for 3D contextual reasoning is critical for recognizing subtle invasion/margin patterns that are frequently missed in 2D slice-based frameworks. Moreover, the multi-level attention design enhances explainability, a key barrier to real-world adoption of deep learning systems in medicine.
Theoretically, the combination of dense connectivity (DenseNet) with hierarchical abstraction (VGG) under attention supervision demonstrates a new approach for large-scale medical imaging tasks where both fine and coarse feature granularity are necessary. The attention visualizations facilitate in-depth error analysis and model interpretability.
Practical applications extend to rapid, accurate stratification of surgical and therapeutic planning, workload reduction for radiologists, and the potential for integration with multi-modal pipelines (e.g., combining MRI with PET or genomic data). The system’s modular design supports straightforward extension to other volumetric medical data contexts (e.g., CT, PET).
Future Directions
Potential improvements include adaptation for pan-modal imaging, incorporation of longitudinal patient data, expansion into multi-site data to further test generalizability, and clinical integration studies. Continued work on attention interpretability is warranted to maximize clinician trust and regulatory compliance. Cross-institutional cloud-based federated learning holds promise for further robustifying performance across heterogenous data sources.
Conclusion
This paper delivers a state-of-the-art hybrid framework combining 3D U-Net segmentation with a DenseNet-VGG classifier, enhanced by multi-head, spatial, and channel attention, achieving superior glioma grading and segmentation performance on MRI data. The empirical results—Dice coefficient of 98% for segmentation and 99.99% classification accuracy—represent a significant advancement over prevailing architectures, establishing new performance baselines for automated glioma grading. The study suggests a promising trajectory for deep learning-driven neuro-oncology workflows, with broad implications for both research and clinical practice.