Physician-Centered Asynchronous Oversight
- Physician-centered asynchronous oversight is a flexible model that decouples real-time physician presence from continuous supervision, maintaining clinical accountability in digital health.
- The approach integrates distributed systems and hierarchical escalation to preserve quality assurance in telemedicine and AI-supported clinical environments.
- Key implementations, including event-driven callbacks, guardrail protocols, and adaptive escalation, have demonstrated up to 40% reduction in oversight time in practical settings.
Physician-centered asynchronous oversight is a paradigm in which physicians maintain clinical accountability and quality assurance over medical processes, patient data, and AI-supported interactions through mechanisms that decouple oversight from real-time presence or direct synchronous supervision. This model is increasingly relevant in distributed healthcare environments, clinical AI deployment, and scalable telemedicine systems, where infrastructure, regulatory boundaries, or workflow pragmatics require flexible, non-continuous forms of expert supervision. The approach incorporates architectural, organizational, and technological strategies that preserve professional standards, safety, and trust in clinical care, even as task execution and intake processes are increasingly delegated to distributed digital systems or non-physician agents.
1. Design Principles and Architectural Models
Key design principles for physician-centered asynchronous oversight can be derived from telemedicine deployments and clinical AI supervision frameworks:
- Social Networks as Incentive Frameworks: Leveraging professional and personal ties among physicians to scaffold accountability and responsiveness, as demonstrated in a Ghanaian remote consultation system that foregrounded colleague and specialty group connections as the core channel for targeted, peer-to-peer case oversight (0801.1927).
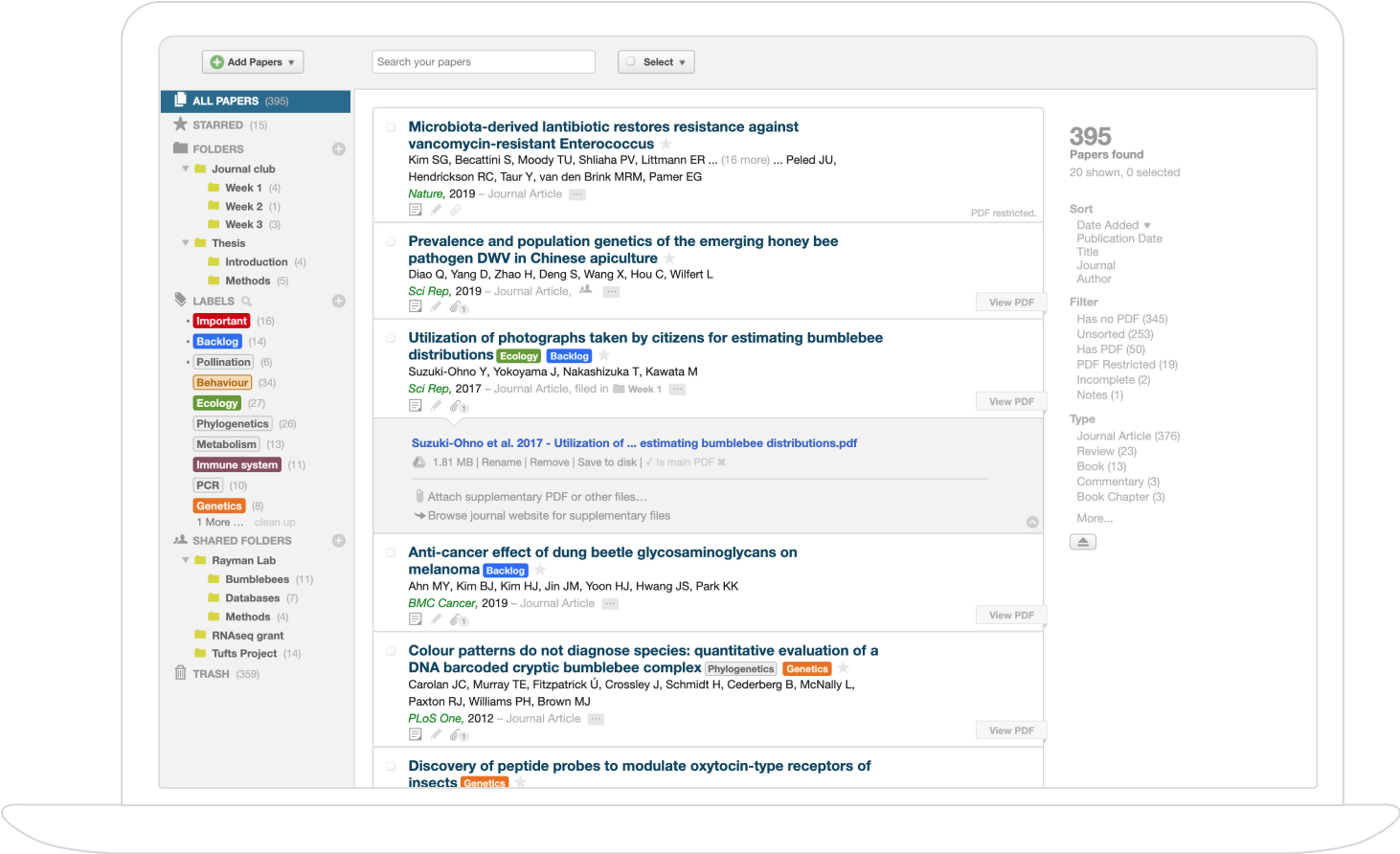
- Optional and Incremental Workflow Integration: Embedding oversight systems as overlays to existing referral and documentation pathways rather than requiring total workflow replacement, enabling gradual, low-friction adoption and sustaining alignment with established clinical culture (0801.1927).
- Weakly-Connected Distributed Architectures: Implementing split interaction models in which local systems (e.g., per-hospital servers, on-device applications) act as synchronous workspaces with asynchronous global synchronization, tolerating unreliable connectivity and facilitating decoupled oversight without loss of data integrity (0801.1927, Shalom et al., 2021).
- Tiered Escalation and Agentic Hierarchy: Employing hierarchical multi-agent systems (such as Tiered Agentic Oversight, TAO), where task complexity and assessed risk dynamically trigger escalation from lower-tier (automated or non-physician) agents to higher-tier, physician-level oversight (Kim et al., 14 Jun 2025).
- Guardrail and Separation-of-Responsibility Protocols: Structuring systems (e.g., g-AMIE) to ensure that intake and history-taking are automated and shielded by a guardrail agent, while individualized advice remains the explicit, accountable domain of the overseeing physician (Vedadi et al., 21 Jul 2025).
2. Implementation Modalities Across Clinical Contexts
Physician-centered asynchronous oversight has been realized in diverse clinical and technological settings:
| Domain | Oversight Modality | Key Implementation/ Metric | |------------------------|-----------------------------------------------|---------------------------------------------------| | Telemedicine for Underserved Settings (0801.1927) | Distributed server overlay, peer consultation | Case data as referral overlay, social group routing, auto-synchronization | | Patient Self-Monitoring (Shalom et al., 2021) | Projection/callback (PCB) model: central & local DSS | Mean time between interactions (e.g., FMTBI=3.95 days for GDM) | | Conversational Diagnostic AI (Vedadi et al., 21 Jul 2025) | Multi-agent intake, physician “cockpit” for review | Quality metrics: SOAP note completeness, time-to-oversight | | Safety Supervision in Clinical AI (Kim et al., 14 Jun 2025) | Multi-tiered agentic oversight, complexity-adaptive escalation | Safety benchmarks: accuracy, harm rates, escalation triggers |
In all cases, asynchronous mechanisms allow physicians to intervene only as needed—either routinely (via periodic case review, notification-driven intervention) or adaptively (via escalation for ambiguities or detected risk).
3. Workflow Dynamics, Incentive Structures, and Trust Coordination
The interplay between trust, efficiency, and oversight cost is central to physician-centered asynchronous models:
- Reputation-Dependent Oversight: Oversight intensity is dynamically tuned to a reputation variable p representing inferred or measured clinical quality. Random audits predominate when trust is high (p > p†), while deterministic, more frequent review and recovery protocols are triggered when trust degrades (p < p†) (Achim et al., 3 Apr 2025).
- Effort-Oversight Substitution and Complementarity: In regimes of high trust, effort (e.g., diligence in documentation or practice) acts as a substitute for oversight; random checks maintain incentives. Conversely, in low trust, oversight and effort become complementary, potentially leading to coordination failures that must be mitigated, for example, by self-disclosure mechanisms (Achim et al., 3 Apr 2025).
- Self-Organizing Growth and Informal Network Activation: Systems that empower physicians to consult through social/professional networks encourage organic oversight, promote self-organizing community effects, and reduce dependency on top-down mandated review (0801.1927).
4. Oversight Mechanisms in AI and Digital Health
Several technical strategies are used to formalize asynchronous oversight over both automated and human agents:
- Call-Back and Event-Driven Models: Decision support tasks are delegated to local devices or non-physician agents, with centralized (physician-level) intervention triggered by event-based callbacks—often determined by guideline violations or anomaly patterns (Shalom et al., 2021).
- Guardrails and Constrained Agents: Automated dialogue or triage agents (e.g., g-AMIE) are programmed with strict guardrails to preclude the delivery of individualized medical advice before review by a human clinician. Turn-level review and constrained decoding enforce regulatory boundaries, with all actionable decisions channelled through asynchronous, accountable physician review (Vedadi et al., 21 Jul 2025).
- Collaboration and Escalation in Multi-Tiered AI: Hierarchical agent systems assign complex, uncertain, or critical cases to higher oversight layers. Safe automation is achieved by consensus and escalation triggers, e.g.,
where indicates an agent's flag for escalation at tier (Kim et al., 14 Jun 2025).
5. Evaluation, Impact, and Limitations
Quantitative and qualitative evaluation of asynchronous oversight frameworks has yielded several findings:
- Clinical Quality and Efficiency: Systems such as g-AMIE demonstrated higher-quality intake, more comprehensive documentation, and increased composite accuracy in diagnostic and management planning, with oversight time reduced by approximately 40% compared to standalone primary care consultations (Vedadi et al., 21 Jul 2025).
- Safety and Error Reduction: TAO outperformed single-agent and conventional multi-agent safety benchmarks by up to 8.2%, particularly when advanced LLMs were assigned to early tiers and robust escalation protocols were enforced (Kim et al., 14 Jun 2025).
- Organizational Scalability: The use of overlays, event-driven escalation, and asynchronous notification protocols allows systems to scale oversight across large catchments or limited-physician settings without proportionally increasing workload (0801.1927, Shalom et al., 2021).
- Challenges: Potential drawbacks include notification gaps due to connectivity failures, synchronization issues between different servers, increased cognitive load from reviewing verbose AI-generated documentation, and difficulties in defining and enforcing guardrail boundaries between authorized and unauthorized advice (0801.1927, Vedadi et al., 21 Jul 2025).
6. Future Directions and Open Problems
Several lines of further investigation are highlighted or implied:
- Integration with EHR and Workflow Systems: Deeper integration with clinical information systems can streamline review, ensure contextual data availability, and support finer-grained escalation criteria (Vedadi et al., 21 Jul 2025).
- Adaptive and Personalized Oversight Calibration: Dynamic tuning of escalation thresholds, reputation updates, and guardrail parameters to physician practice patterns, clinical context, and real-world event distributions (Achim et al., 3 Apr 2025, Kim et al., 14 Jun 2025).
- Explainability and Transparent Oversight: While alignment of AI explanations (e.g., attention maps) with physician judgment is proposed as a meta-information channel, empirical evidence suggests that such alignment alone may not reduce uncertainty or improve trustworthiness, calling for inherently interpretable or ante hoc explainability solutions (Kobayashi et al., 2023).
- Community-Driven Training and Feedback Loops: Continuous provider feedback, crowd-sourcing of oversight calibration, and self-organizing network enhancements to foster sustainable adoption and quality improvement (0801.1927).
- Hybrid and Cross-Disciplinary Teams: Integration of agentic, automated oversight with clinician-in-the-loop review, wherein complex or ambiguous cases are flagged and routed for expert analysis, maximizing safety and system adaptability in high-stakes clinical environments (Kim et al., 14 Jun 2025).
Physician-centered asynchronous oversight thus constitutes an increasingly essential organizational and technical principle for scalable, safe, and efficient supervision of complex healthcare delivery—particularly as digital health, telemedicine, and AI-driven systems proliferate in varied clinical environments.