Deep Learning for Clinically Relevant Segmentation of Head and Neck Anatomy in Radiotherapy
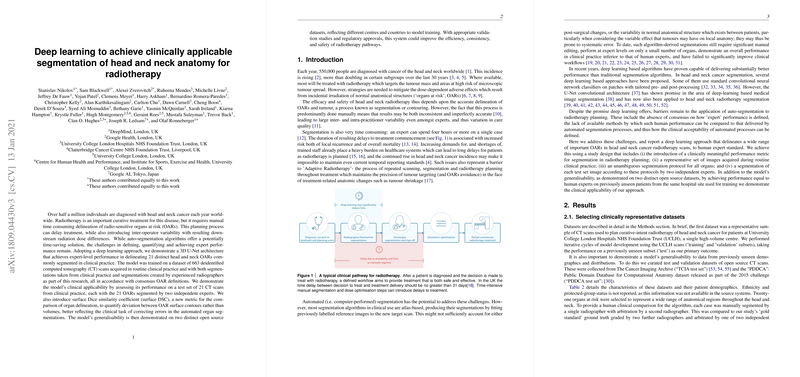
The paper Deep learning to achieve clinically applicable segmentation of head and neck anatomy for radiotherapy presents a comprehensive paper aimed at tackling the challenges of automating organ segmentation in the context of radiotherapy for head and neck cancer. This research utilizes a deep learning architecture, specifically a 3D U-Net model, to achieve expert-level performance in the segmentation of 21 organs at risk (OARs). The aim is to enhance the efficiency, consistency, and safety of radiotherapy treatments by providing reliable automated segmentations that can reduce the variability and time demands associated with manual delineation.
Methodology and Experimental Design
The paper employs a dataset composed of 663 CT scans for the model's training, which includes segmentations derived from clinical practice as well as those manually created by trained radiographers. For evaluation, the model's performance was tested against a separate set of 21 CT scans, each manually segmented by two independent experts, and further validated across two open-source datasets reflecting differing demographics and imaging protocols.
A significant methodological contribution is the introduction of the surface Dice similarity coefficient (surface DSC) metric. Unlike traditional volumetric DSC, the surface DSC evaluates the overlap of OAR surface contours, thus providing a metric more aligned with the clinical task of error correction in automated segmentation. This metric reflects human effort in redrawing segmentation boundaries during clinical workflows, offering a finer-grained performance assessment, particularly pertinent for radiotherapy applications.
Results and Performance Analysis
Quantitatively, the model demonstrates high accuracy in segmenting multiple OARs, achieving performance comparable to experienced radiographers. The surface DSC for the automated segmentations closely matched manual annotations, with notable scores on several critical structures. The model was also subjected to rigorous testing across curated datasets from distinct geographic locations (including the TCIA and PDDCA datasets) to verify its robustness and generalizability.
This research underscores several technical accomplishments:
- Generalizability: The deep learning model maintained high performance levels across diverse test sets, involving data from different countries and clinical settings, emphasizing robustness in varying imaging conditions.
- Clinical Relevance: The introduction and application of the surface DSC metric provide a new benchmark for evaluating segmentation tasks in radiotherapy, bridging the metric with actual clinical demands and efforts in post-processing automated outputs.
- Efficiency: Through automation, the segmentation process for head and neck anatomy can potentially be expedited, leading to more timely radiation therapy planning and potentially reducing the risk of treatment delays.
Implications and Future Directions
The implications of this research are vast, as the automated segmentation model could greatly streamline the radiotherapy planning process by minimizing time-intensive manual segmentation and inter-operator variability. This, in turn, could improve overall treatment quality and patient outcomes. Furthermore, the novel surface DSC metric has the potential to become a standard in evaluating medical image segmentation due to its closer alignment with clinical practice.
Future research areas could explore the integration of other imaging modalities such as MRI, expanding the range of delineable structures, and further refining the surface DSC metric as consensus around its clinical efficacy grows. Additionally, exploring integration with adaptive radiotherapy processes to accommodate anatomical changes over treatment courses is a promising direction.
Ultimately, with continued validation and adherence to rigorous regulatory standards, the deployment of such automated systems in clinical settings could mark a significant step toward enhancing radiotherapy pathways for head and neck cancer patients.